When Should a Practice Outsource Medical Billing?
Medical billing is the financial backbone of any healthcare practice. Done right, it keeps cash flow steady, claims moving, and patients satisfied. Done poorly, it creates delays, denials, and unnecessary overhead. Many providers face the same question: when should a practice outsource medical billing?
Outsourcing medical billing can streamline operations, cut costs, and free up staff to focus on patient care—but it’s not always the right move for every practice. Below, we’ll break down the key signs that indicate when it’s time to consider outsourcing.
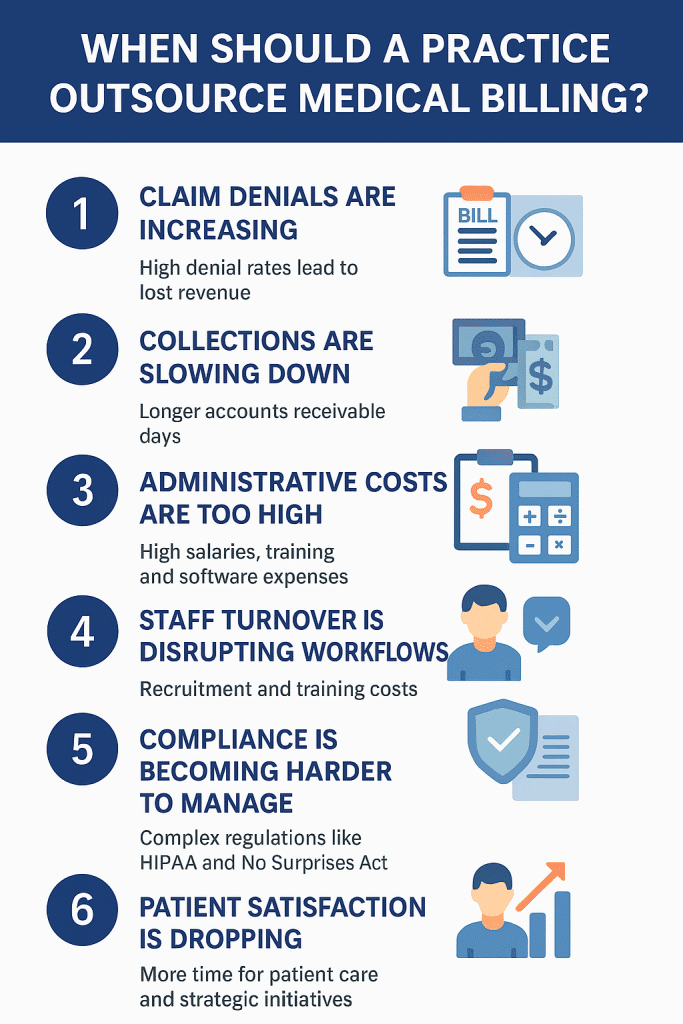
1. Claim Denials Are Increasing
If you’re noticing a higher-than-average denial rate, that’s a red flag. Denials usually happen due to coding errors, missed deadlines, or incomplete patient data. Even a small percentage of denied claims can mean tens of thousands in lost revenue annually.
An outsourced billing partner has teams dedicated to denial management. They know the nuances of CPT, ICD-10, and payer-specific requirements—ensuring claims are clean the first time and quickly corrected if denied. If your staff is struggling with repetitive claim rework, it may be time to outsource medical billing.
2. Collections Are Slowing Down
Cash flow is critical for stability. When accounts receivable (A/R) days creep past 30–45, practices start to feel the squeeze. Slower collections often happen because:
-
Claims aren’t submitted promptly
-
Staff don’t have the bandwidth to follow up with payers
-
Denials sit unresolved
-
Patient balances aren’t pursued consistently
The result? Cash flow bottlenecks that put pressure on payroll, rent, and supply costs.
When a practice outsources medical billing, dedicated billing teams track claims from submission through payment. They chase down unpaid balances, appeal denials, and establish consistent patient billing processes. Outsourcing also allows practices to use advanced billing software that provides better reporting, so you can track financial performance in real time.
If reimbursements are slowing down and A/R is climbing, outsourcing may be the fastest way to restore a healthy revenue cycle.
3. Administrative Costs Are Too High
Running an in-house billing department isn’t just about salaries. You’re also paying for benefits, ongoing training, office space, software licenses, and IT support. Add in costs for compliance audits and turnover, and the overhead can quickly outweigh the benefits of keeping billing internal.
With outsourcing, you typically pay a predictable percentage of collections, which eliminates fluctuating costs and makes budgeting easier. This can free up capital to reinvest in staff development, patient care, or new service lines.
4. Staff Turnover Is Disrupting Workflows
Billing staff are highly specialized, and when one leaves, it often disrupts the entire revenue cycle. Recruiting, hiring, and training replacements takes time—and during that gap, claims pile up.
Outsourced billing ensures continuity. Vendors have trained professionals on standby, so your practice never experiences downtime due to staffing issues. For practices with limited HR resources, this stability can be a game changer.
5. Compliance Is Becoming Harder to Manage
Healthcare regulations are constantly evolving—HIPAA, Medicare and Medicaid guidelines, payer-specific requirements, and laws like the No Surprises Act all affect billing. Staying compliant requires constant training and frequent policy updates.
For many practices, compliance becomes unmanageable when billing is handled in-house by a small team. Mistakes can lead to costly penalties, audits, or even accusations of fraud.
When you outsource medical billing, you gain access to experts who monitor regulatory changes daily. Reputable billing partners also implement secure technology, conduct compliance audits, and follow best practices for protecting patient data. This not only reduces risk but also gives providers peace of mind that compliance isn’t falling through the cracks.
If you find your staff struggling to keep up with compliance or worrying about exposure to audits, that’s a strong sign your practice should outsource medical billing.
6. Patient Satisfaction Is Dropping
Confusing bills, unclear insurance explanations, and delayed statements frustrate patients. If your front desk team spends more time fielding billing complaints than scheduling appointments, patient satisfaction suffers.
Outsourced billing partners often provide patient-friendly statements, online payment portals, and customer support for billing questions. This reduces the burden on your in-house staff and makes the billing process more transparent for patients—improving both satisfaction and trust.
7. You Want to Focus on Growth, Not Paperwork
One of the biggest hidden costs of in-house billing is the distraction it creates. Doctors, managers, and administrative staff often get pulled into billing issues—appealing denials, reviewing reports, or training staff. Over time, this takes energy away from strategic initiatives like expanding services, adding new locations, or improving patient experience.
Outsourcing medical billing allows practices to reallocate time and resources. Instead of spending hours each week managing claims, leaders can focus on:
-
Developing new service lines or procedures
-
Expanding into new markets or locations
-
Investing in patient engagement and retention
-
Building referral networks and partnerships
Ultimately, practices that outsource medical billing position themselves for growth. They gain the freedom to think strategically instead of getting stuck in the weeds of daily billing problems.
Conclusion
So, when should a practice outsource medical billing? The answer is clear if you’re seeing rising denials, slower collections, compliance headaches, or if your leadership team feels bogged down by billing. Outsourcing isn’t just about saving money—it’s about improving efficiency, strengthening cash flow, reducing risk, and creating space to focus on what matters most: patient care and practice growth. With Aspire Health Management, outsourcing medical billing feels seamless—like it’s still in-house—because we fight for every dollar with insurance companies and maintain clear, consistent communication with you throughout the process. Contact us today for a free business evaluation and see how you practice can succeed like never before.