What is Revenue Cycle Management
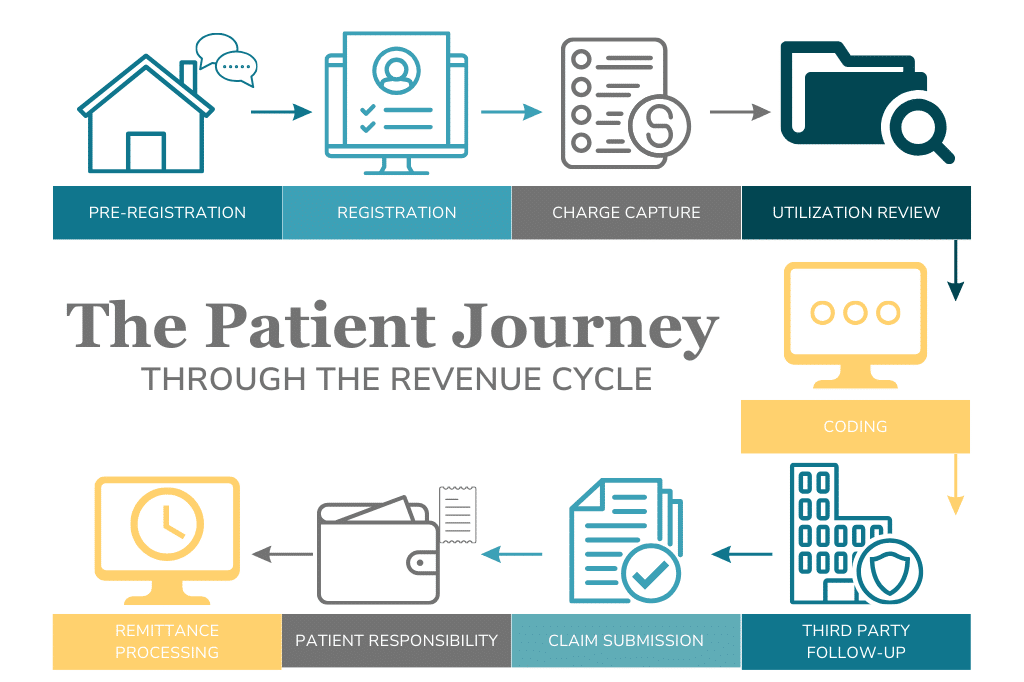
Revenue Cycle Management (RCM) is a critical process that begins with the first interaction between a healthcare provider and a patient. This journey, from verifying insurance and scheduling appointments to clinical care and billing, involves multiple steps and requires coordination among various departments. Ensuring a seamless RCM system not only enhances financial performance but also improves patient satisfaction. Here, we explore the nine essential steps of the billing cycle and the need for seamless communication between the different teams and roles in order to have successful RCM.
1. Pre-Registration (Front Office Team)
The RCM journey starts with pre-registration, where the front office team gathers as much information as possible about the patient and their insurance. This step ensures that the patient is eligible for the services and is scheduled with the appropriate provider at the right location. Leveraging technology, such as Practice Management (PM) software or third-party scheduling tools, can expedite administrative tasks and improve accuracy.
2. Registration (Front Office Team)
During registration, the front office team collects any remaining patient information and necessary consents. This is an opportunity to engage patients, inform them about their financial obligations, and educate them on the next steps of their care. Ensuring eligibility checks and collecting co-pays at this stage is crucial. Technology such as, patient portals or e-documents can streamline the process, reducing the burden on staff and enhancing patient convenience.
3. Charge Capture (Clinical Team)
Charge capture involves recording the services provided by clinicians, which are then used to generate medical claims for billing. Accurate documentation is essential to avoid revenue loss or issues during audits. Clinicians should use templated charge slips with built-in codes to ensure efficiency and correctness. Proper documentation directly impacts the financial health of the organization.
4. Utilization Review (Clinical Team)
Utilization review is an ongoing process where providers assess their treatment plans to ensure they are medically necessary, cost-effective, and aligned with industry best practices. This step not only helps in reducing unnecessary costs but also improves patient outcomes by adhering to standardized care protocols.
5. Coding (Billing Team)
Specialized coders audit the medical diagnoses and procedures documented by the clinical team. Accurate coding is vital as it determines the payment from insurers. Coders must stay updated with current practices and certifications to ensure compliance and accuracy. They play a key role in identifying and correcting coding issues, thereby optimizing revenue.
6. Third-Party Follow-Up (Billing Team)
The billing team is responsible for pursuing payments from third-party payers. This step is crucial because federal regulations mandate that Medicaid and Medicare are payers of last resort. Efficient third-party follow-up ensures that all possible avenues are explored before billing government programs, maximizing revenue from private insurers who typically pay higher rates. A good billing team is the difference between collecting 70% vs collecting 95%
7. Claim Submission (Billing Team)
Submitting clean claims – those that are accurate and complete – to insurance companies is essential for timely reimbursement. Consistent and accurate coding reduces errors and claim denials. The billing team must be persistent in reworking denials and communicating with the clinical team to refine billing practices continually.
8. Patient Responsibility (Front Office and Billing Team)
When insurance does not cover the entire bill, patients are responsible for the remaining balance. Educating patients on their financial responsibilities and offering assistance with billing concerns are crucial. The front office team should address basic billing inquiries, while more complex issues can be referred to the billing team. Clear communication and support can significantly enhance patient satisfaction.
9. Remittance Processing (Billing Team)
This is another area where the billing team needs to work closely with the clinical and front office teams for timely billing and appealing denials. Once payments are received, they must be accurately allocated to the patient’s account. Timely billing is critical as different payers have specific deadlines. The billing team should have a structured process for sending statements and handling non-responsive patients, including potential collection notices. Helping patients navigate financial assistance options can also be part of this step.
The Importance of a Cohesive RCM System
A successful RCM system is not solely the responsibility of the billing team. It requires coordinated efforts across various departments, each maintaining high levels of communication and competency. The billing experience is integral to a patient’s overall experience with a healthcare provider and can influence their decision to return or recommend the provider to others. A 2021 study done by PYMNTS found that 63% of patients would switch their healthcare provider if they had a negative billing experience.¹
Continuous training and support from the billing team to the clinical and front office staff are essential. Instead of relying on the billing team to fix all mistakes, each team member should be accountable for their errors, fostering an environment of continuous improvement.
In conclusion, an effective RCM system enhances the financial health of a healthcare organization while ensuring excellent patient care. By following these nine steps and fostering collaboration among teams, healthcare providers can achieve a streamlined and efficient revenue cycle management process.
If your organization is ready to optimize its revenue cycle management, then take the first step towards enhanced efficiency and improved patient satisfaction today. Contact us today to learn how our comprehensive RCM solutions can transform your billing process and drive financial success. Let’s work together to achieve excellence in every aspect of your healthcare services. Reach out now to schedule a consultation and start your journey towards a more effective RCM system.
¹“The Payment Cure: How Improving Billing Experiences Impacts Patient Loyalty.” 2021. PYMNTS.Com. CareCredit. September 2021. https://www.pymnts.com/wp-content/uploads/2021/09/PYMNTS-The-Payment-Cure-September-2021.pdf.


